
You may have heard your provider or fellow POTSies refer to subtypes of POTS, like hypovolemic, hyperadrenergic, and neuropathic. However, not all autonomic specialists agree that there are distinct subtypes of POTS or that they’re worth differentiating.
We recently asked our Instagram community what they wanted to know about this widely debated topic and shared their questions with researcher and POTS patient, Dr. Amanda Miller, Ph.D.
Amanda Miller, Ph.D. is a scientist who has studied POTS, neural control of blood flow, and cognitive dysfunction for 12 years. Dr. Miller obtained a Ph.D. in neuroscience in 2017 and her goal is to discover mechanisms and novel therapeutics for POTS and related chronic illnesses. Dr. Miller has published several research papers on POTS and serves on the Board of the American Autonomic Society and the Dysautonomia International Patient Advisory Board.
“It's not surprising that this topic is unclear to people with POTS since experts treating POTS do not agree on criteria for POTS subtypes or whether the subtypes even exist...” Dr. Miller said. “So, there are no short and simple answers.”
Here is what Dr. Miller had to say.
Q: Is there actually a distinct difference in POTS subtypes?
A: “Like I said before, opinions on this topic differ but based on most of the evidence, my short answer is no, the subtypes of POTS are not distinct. Furthermore, it is possible to have both hyperadrenergic and neuropathic POTS as well as hypovolemic, post-viral, or any other suggested subtype. These are not mutually exclusive, and it is possible for a person with POTS to have all or none of the described subtypes.
The three main POTS subtypes described in the literature are hypovolemic, hyperadrenergic, and neuropathic POTS.
Hypovolemic POTS probably applies to most people with POTS and is not a distinct subtype. Hypovolemia is not easy to measure or diagnose, but most people with POTS have symptoms of hypovolemia and significant improvement with volume expansion via IV hydration.”
Hypovolemia can be defined as low levels of fluids, like blood volume, in the body that causes a disruption in the body’s balance of internal processes.
“Hyperadrenergic POTS is characterized by resting tachycardia, orthostatic hypertension, excessive sweating, cold hands and feet, tremors and anxiety. The hyperadrenergic diagnostic criteria is based on excess catecholamines while upright. Some criteria state that plasma norepinepherine (NE) >1000pg/mL suggests hyperadrenergic POTS. Yet other state NE over 600 pg/mL is hyperadrenergic. Most POTS patients meet the NE >600 pg/mL criteria and many who have the hyperadrenergic presentation (high blood pressure and resting tachycardia) don't meet the 1000pg/mL criteria so neither criteria is selective nor specific to hyperadrenergic POTS.
For neuropathic POTS, [there are] many patients with low blood pressure, excessive blood pooling in the abdomen and legs, lack of sweating, and presyncope. The symptoms of neuropathic POTS are consistent with small fiber neuropathy. However, about half of patients with the neuropathic subtype will not have neuropathy confirmed by QSART or a skin biopsy. Patients with neuropathic symptoms might have high plasma norepinephrine during tilt table despite not meeting the hyperadrenergic phenotype.”
Q: Is it important to know what subtype I have? If so, how do I find out?
A: “[T]he tests are not specific or selective to diagnosing a phenotype, and many people with POTS overlap phenotypes. Additionally, the tests for hyperadrenergic and neuropathic POTS are not readily available and can cost thousands of dollars in out-of-pocket medical costs as well as travel to an autonomic neurologist or neurophysiologist.
...I understand that importance is subjective. We all want answers and if you have the means to acquire more testing, it could be beneficial to understanding your symptoms and guiding treatment.”
Q: How do management strategies/treatments differ for the different subtypes of POTS, especially hyperadrenergic POTS?
A: “There are some studies (including one of mine on midodrine) that have observed different effects to treatments in neuropathic and hyperadrenergic POTS. However, most treatments are trial and error and don't rely solely on subtype. Things like [blood] volume expansion and exercise are recommended for all POTS patients. There are suggestions that vasoconstrictors may work better in neuropathic POTS while adrenergic blockers are more beneficial in hyperadrenergic presentation, however, there isn't a lot of data to back these claims. In addition, a certain diagnosis of hyperadrenergic vs. neuropathic POTS is not necessary to guide treatment. Discussing your POTS symptoms with your doctor and suggesting a certain therapeutic course is sufficient.”
Below is a diagram from a review that Dr. Miller wrote with Dr. Satish Raj on pharmacotherapy for POTS published in 2018 in Autonomic Neuroscience.
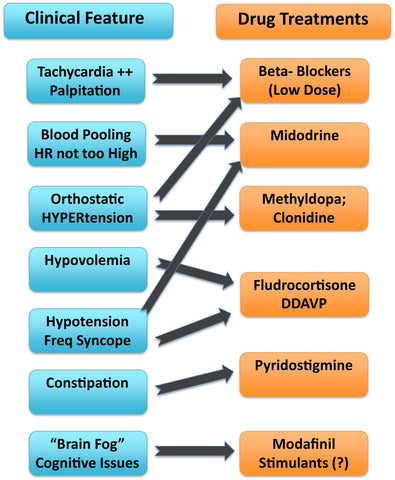
POTS patients may have overlapping subtypes or may not have a known subtype at all. Please consult your healthcare provider to determine what route and treatment options are best for you.
Q: Do you have any tips for working out with hyperadrenergic POTS?
A: “Advice for working out with hyperadrenergic POTS is similar to the advice for any person with POTS. I view exercise as a treatment strategy that helps some people manage their symptoms. Exercise is not a cure, it doesn't help everyone, and like any treatment — there are side effects. However, most people with POTS should try an exercise program because exercise can have robust effects on the heart and brain and significantly reduce POTS symptoms including tachycardia, fatigue, and brain fog. It's important to manage symptoms with pharmacological and non-pharmacological approaches in order to tolerate exercise and avoid post-exertional fatigue.
For those with hyperadrenergic POTS, it may be more important to regulate heart rate first with a beta-blocker, mestinon, or ivabradine prior to initiating exercise. Volume expansion with oral or IV fluids and electrolytes may also be necessary. Exercise should also be started low and slow and gradually increased as tolerated in accordance with guidelines for POTS.”
See more about exercise recommendations for POTS from Dysautonomia International.
If you would like to learn more, new research from Mayo Clinic found that the subtypes of POTS are indistinguishable by symptoms and many patients experience overlapping subtypes.
Note: This Q&A is intended for informational purposes only and is not intended to treat or diagnose any medical condition or provide medical advice. Please consult your healthcare provider for any questions you may have or before you begin any medical treatments.







